
▲全球视界 本乡考虑
★专业/深度/睿见资讯尽在医疗游览
世界卫生安排发布了关于调整下一阶段COVID-19应对办法的公共卫生和社会办法的辅导定见。它正告说,签发“豁免护照”或“无危险证”以使个人能够游览是危险的。
一些政府主张,对引发COVID-19疾病的病毒抗体检测,可当作答应个人游览或重返工作岗位的“免疫护照”或“无危险证明”的根底,假定他们能遭到维护避免再次感染。
世界卫生安排指出,没有依据标明从COVID-19中康复过来并具有抗体的人能够免受第2次感染。
经过天然感染对病原体发作免疫是一个多进程进程,一般需求1-2周。人体对病毒感染的反响是一种非特异性先天反响,其间巨噬细胞,中性粒细胞和树突状细胞能够减缓病毒的进程,还能够阻挠病毒引起症状。这种非特异性反响之后是习惯性反响,在这种习惯性反响中,人体发作与病毒特异性结合的抗体。这些抗体是称为免疫球蛋白的蛋白质。人体还制作T细胞,然后辨认并消除感染病毒的其他细胞。这称为细胞免疫。
这种组合的习惯性反响能够铲除体内病毒,假如反响满足激烈,能够有用的防备发展为严峻疾病或再次感染同一病毒。这样的一个进程一般是经过血液中抗体的存在来衡量的。
世卫安排持续检查有关抗体反响的依据,大多数研讨标明,从感染中康复过来的人都具有该病毒的抗体。可是,其间一些人的血液中的中和抗体水平很低,这标明细胞免疫关于康复也或许至关重要。
现在还没有研讨评价这种病毒的抗体,即严峻急性呼吸综合征冠状病毒2(SARS-CoV-2)的存在是否会对这种病毒随后在人体内的感染发作免疫力。
检测人体中SARS-CoV-2抗体的实验室检测,包含快速免疫诊断实验,需求进一步验证,以确认其是否精确牢靠。不精确的免疫诊断实验或许会以两种方法对人进行过错的分类。一是或许过错地将感染者标记为阴性,二是未感染者被过错地标记为阳性。这两个过错都有严峻后果,并将影响操控尽力。
这些测验还需求精确区别曩昔的SARS-CoV-2感染和已知的6种人类冠状病毒引起的感染。这6中病毒中有4种会引起一般伤风并广泛传达。其他2种是引起中东呼吸综合症和严峻急性呼吸综合症的病毒。被这些病毒中的任何一种感染的人所发作的抗体或许会与针对SARS-CoV-2感染而发作的抗体发作穿插反响。
许多国家/区域正在根底人群或特定人群中(如卫生工作者,已知病例的密切触摸者或家庭内部)检测SARS-CoV-2抗体。世卫安排支撑这些研讨,因为它们关于了解感染的程度和危险要素至关重要。这些研讨将供给可检测到COVID-19抗体的人的百分比数据,但大多数研讨并不是为了确认这些人是否对继发感染免疫。
在大盛行的这一点上,没有满足的依据证明抗体介导免疫的有用性,以确保“免疫护照”或“无危险证明”的精确性。因为检测成果呈阳性而以为自己对第2次感染免疫的人,或许会忽视公共卫生主张。因而,运用这种证书或许会添加持续传达的危险。*
WHO WARNS AGAINST ‘FREE OF COVID-19’ CERTIFICATES
The World Health Organization (WHO) has published guidance on adjusting public health and social measures for the next phase of the COVID-19 response. It warns that issuing an ‘immunity passport’ or ‘risk-free’ certificates to enable individuals to travel are dangerous.
Some governments have suggested that the detection of antibodies to the virus that causes the disease COVID-19, could serve as the basis for an “immunity passport” or “risk-free certificate” that would allow individuals to travel or to return to work, on the assumption that they are protected against re-infection.
The WHO states that there is no evidence that people who have recovered from COVID-19 and have antibodies are protected from a second infection.
The development of immunity to a pathogen through natural infection is a multi-step process that typically takes place over 1-2 weeks. The body responds to a viral infection immediately with a non-specific innate response in which macrophages, neutrophils, and dendritic cells slow the progress of virus and may even prevent it from causing symptoms. This non-specific response is followed by an adaptive response where the body makes antibodies that specifically bind to the virus. These antibodies are proteins called immunoglobulins. The body also makes T-cells that recognise and eliminate other cells infected with the virus. This is called cellular immunity. This combined adaptive response may clear the virus from the body, and if the response is strong enough, may prevent progression to severe illness or re-infection by the same virus. This process is often measured by the presence of antibodies in blood.
The WHO continues to review the evidence on antibody responses and most studies show that people who have recovered from infection have antibodies to the virus. However, some of these people have very low levels of neutralising antibodies in their blood, suggesting that cellular immunity may also be critical for recovery.
No study has evaluated whether the presence of antibodies to the virus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), confers immunity to subsequent infection by this virus in humans.
Laboratory tests that detect antibodies to SARS-CoV-2 in people, including rapid immunodiagnostic tests, need further validation to determine their accuracy and reliability. Inaccurate immunodiagnostic tests may falsely categorise people in two ways. The first is that they may falsely label people who have been infected as negative, and the second is that people who have not been infected are falsely labelled as positive. Both errors have serious consequences and will affect control efforts.
These tests also need to accurately distinguish between past infections from SARS-CoV-2 and those caused by the known set of six human coronaviruses. Four of these viruses cause the common cold and circulate widely. The remaining two are the viruses that cause Middle East Respiratory Syndrome and Severe Acute Respiratory Syndrome. People infected by any one of these viruses may produce antibodies that cross-react with antibodies produced in response to infection with SARS-CoV-2.
Many countries are testing for SARS-CoV-2 antibodies at the population level or in specific groups, such as health workers, close contacts of known cases, or within households. The WHO supports these studies, as they are critical for understanding the extent of and risk factors associated with infection. These studies will provide data on the percentage of people with detectable COVID-19 antibodies, but most are not designed to determine whether those people are immune to secondary infections.
At this point in the pandemic, there is not enough evidence about the effectiveness of antibody-mediated immunity to guarantee the accuracy of an “immunity passport” or “risk-free certificate.” People who assume that they are immune to a second infection because they have received a positive test result may ignore public health advice. The use of such certificates may therefore increase the risks of continued transmission.

 万众瞩目:络病大会召开 微血管病变防治开辟新局面
万众瞩目:络病大会召开 微血管病变防治开辟新局面 毓婷x学院奖云课堂完美收官|“毓”青春同行,创意步履不“婷”
毓婷x学院奖云课堂完美收官|“毓”青春同行,创意步履不“婷”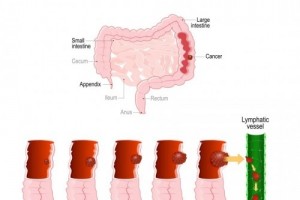 发现就是中晚期的结直肠癌,其实有办法可以避免!
发现就是中晚期的结直肠癌,其实有办法可以避免! “毓”见别YOUNG青春——毓婷携手学院奖2022再启新程
“毓”见别YOUNG青春——毓婷携手学院奖2022再启新程 成都中德肾病医院付冬梅--专业经验技术 让你放心无忧
成都中德肾病医院付冬梅--专业经验技术 让你放心无忧 成都中德肾病医院专家韩艳简介
成都中德肾病医院专家韩艳简介 屈燧林--成都中德肾病医院特聘专家
屈燧林--成都中德肾病医院特聘专家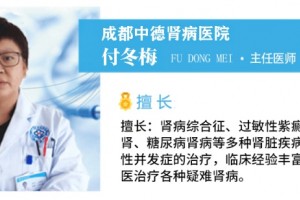 成都中德肾病医院付冬梅主任:糖尿病肾病应该如何治疗与调养
成都中德肾病医院付冬梅主任:糖尿病肾病应该如何治疗与调养